Chronic Pain affects 100,000 people in the U.S. and is a leading reason people seek treatment from doctors. Many people, including MD's, are unaware that there are alternatives to narcotic and medication-based treatments. Exercise is one of the best, but it should be started gradually.
Chronic pain is defined as pain that lasts more than three to six months. It usually is expressed in back pain, headaches, and shoulder or neck pain. There are many things that can contribute to the chronic pain such as decreased strength, increased muscle tightness, joint tightness, joint pain, muscle balance disturbances, postural changes, gait changes, and generalized deconditioning.
Physiologically, chronic pain is not just a symptom, but a transformation of the nervous system. The body no longer needs injury to trigger pain, the revved-up nerves do it all by themselves. Without intervention to manage it, chronic pain continues to get worse, making the nervous system more and more sensitive.
The Fear-Avoidance Model refers to how a patient avoids an activity that he/she believes will cause or worsen pain. The inactivity leads to further pain, leading to further avoidance, etc. This cycle creates a chronic pain condition. By breaking the cycle, pain can be lessened and often alleviated.
At CHPT, we have a comprehensive program to teach you how to decrease the pain you have and to prevent and manage pain flare-ups. Our techniques include the appropriate use of heat and cold, proper stretching and exercises.
Q: How does pain become chronic?
A: Everyone's nervous system is different, and people perceive pain in different ways. Pain sensors are found in every part of our body and are connected to nerves. The nerves send a signal to the brain, which tells us that we are feeling; pain is a signal that tissues in the body are in danger of injury. When the body continually senses pain for a long period of time, it sends messages that the body is in danger, even when there is no longer tissue damage. For example, most movements should not hurt us. But for people in chronic pain, the brain actually changes the message, perceiving simple movements or light touch as pain. Long term, it takes fewer and fewer sensors activated to feel pain.
Q: Why do I feel more pain when I'm stressed?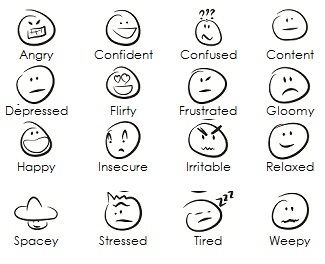
A: Pain perception shares neuropathways with cognition and emotion. Stress can amplify pain.
According to the book Explain Pain by Dr. Lorimer Moselely, our emotions, stress and attitude can change our pain. Stress can produce chemicals to activate danger messages in our nerves, which then makes our brain produce more stress chemicals, and it becomes a vicious cycle. Numerous studies have shown that stress can amplify the effects of chronic pain. Pain and emotion are like a door that swings both ways: anxiety and depression can increase pain, and increased pain can cause a rise in depression and anxiety.
Q: What can I do to help myself manage chronic pain?
A: Active self-management is the key to improvement.
Remember that most of the tissues in our body are tougher than we think; you cannot hurt them by moving more, even though it hurts. As long as you are staying within your tolerance, you will find that you feel much better after movement. Your physical therapist can give you feedback to help you interpret what is helpful and what is too much.
Q: What about relaxation techniques?
A: Relaxation techniques can help you manage stress levels.
Certain exercises and relaxation techniques can be used during a flare-up. It is important during a flare-up to have self-management techniques to calm the area and your whole body so you can get on with the rest of your day. Knowing these in advance and practicing them with your physical therapist will increase your confidence to manage flares on your own.
